Shortly after Charles Knuckles passed out while trying to hang himself in a heroin-induced stupor, he walked several blocks to Cityteam, a faith-based shelter for the poor and homeless in Chester, Pennsylvania. He looked so beat up that the receptionist advised him to leave. “Mister, I don’t know what to do with you,” Knuckles recalls being told. “So I sat down and said, ‘Lady, I can’t go—I’m going to die.’”
Knuckles survived—thanks to the shelter’s director, who took him in and helped him overcome his drug addiction. An African American who was orphaned at the age of two and was an addict for 30 years, he went on to become the shelter’s director. Now 67 years old, he heads a Cityteam recovery center in San Jose, California. The facility houses 72 recovering addicts and 56 homeless people, serving them 600 meals daily and helping them with everything from medical and dental care to substance use counseling and job placement.
Were Knuckles to have the same near-death experience today, 18 years later, chances are he probably wouldn’t find a treatment facility that would have had the same outcome for him, even though the nation has more than 14,500 specialized drug treatment facilities, according to the National Institute on Drug Abuse (NIDA). Recent estimates from the federal Substance Abuse and Mental Health Services Administration show that of the 23.1 million Americans who needed treatment for alcohol or drug problems in a single year, only 2.5 million (about 11 percent) received aid at a specialty facility. Partly as a result of that gap, nearly half a million Americans died of drug overdoses from 2000 to 2014, mostly from opioid painkillers and heroin.
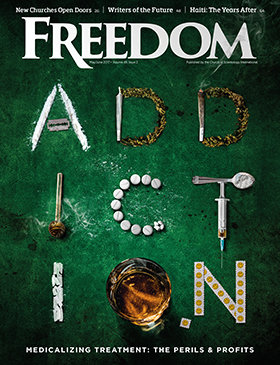
The truth is that substance use addiction is the nation’s most neglected health crisis, afflicting more people than those with heart disease, diabetes or cancer. And the problem is getting worse every day because of healthcare policies and business models that are turning a blind eye to people’s suffering.
Let’s say you have an addiction issue and want to sign up for an abstinence treatment program where you won’t be given any drugs of any sort, not even medications that might leave you feeling drowsy and sluggish. You’re fortunate enough to have reasonably good health insurance; your policy covers 30 days of inpatient treatment. But because hardly anyone gets all 30 days covered these days, your insurer tells you that your coverage will be no more than two weeks. And then he drops a bomb: That wellness program you have in mind is not covered under your plan—or any other plan for that matter—because it’s drug free. You’re welcome, however, to join a program where you’ll be shot up with medications as a detox service. It’s either that, you quickly realize, or you are denied the program of your choice.
Welcome to medication-assisted treatment (MAT), an increasingly influential and controversial paradigm in the world of medicine that, among other things, considers addiction a chronic “brain disease” rather than a condition that can be treated by addressing the social and spiritual aspects underlying addiction. The term refers to the practice of giving patients slow-acting opioids that bind to brain receptors and cause a biological reaction. These opioids are approved by the Food and Drug Administration (FDA) to manage patients’ painful withdrawal symptoms or detoxify them.
MEDICAL MADNESS?
The treatment of drug addiction by administering yet more potentially addictive drugs isn’t just profoundly counterintuitive. It is also a case of bad science and flawed policy: nearly half of all opioid overdose deaths in the United States involve prescription medications. That’s at least 45 Americans every day, given that 91 people in the U.S. die daily from an opioid overdose, according to the Centers for Disease Control and Prevention.
Unlike abstinence-based programs, the pharmacological treatment of addiction is stigmatizing. Methadone, which is used today by more than 250,000 Americans, making it the most widely used medication for treating heroin addiction, is available only at specially licensed “maintenance clinics” where people wait in long lines to get their pills.
Methadone also carries a high risk of death from accidental overdose, especially during the initial stages of treatment, because it tends to suppress the respiratory system. And in what is one of the most glaring examples of double standards in modern medicine, the medication is freely dispensed from doctors’ offices for the treatment of pain, without any licensure, thereby exacerbating the nation’s opioid addiction epidemic. (In fact, it is the prescription of methadone for pain—not methadone from maintenance clinics—that has been a major contributor to the nation’s high opioid painkiller overdose death rates over the past two decades.)
Psychiatry’s “bible” for diagnostics, which insurance companies rely on for billing treatments, dropped the use of two long-running umbrella terms—“substance abuse” and “substance dependence”—replacing them with no less than six “substance use disorders.”
Another medication, Suboxone, a combination of two different drugs that comes in the form of a film rather than a pill, has been hailed for having one distinct advantage over methadone: Doctors can prescribe a month’s supply, thereby eliminating the need for daily visits to clinics. Further, the medication does not have the same risk of accidental overdose. But this “blockbuster” medication, as The New York Times once called it, has spawned its own epidemic, requiring its own pharmacological treatment.
Among other things, MAT is based on the reasoning that just as diabetes is a disease of the pancreas, addiction is a disease of the brain. “It’s completely ideological, conceptually confused and terribly misleading,” says Sally Satel, a psychiatrist and resident scholar at the American Enterprise Institute for Public Policy Research, a conservative think tank in Washington, D.C., and a lecturer at the Yale University School of Medicine. “To reduce something as complicated as addiction to brain functioning, which of course is part of it, deprives you of so much information about why people start getting addicted, why they continue and why they stop.
“The implications of thinking about addiction in such a reductionist and medicalized way tends to de-emphasize the more important elements of addiction that take place at the psychological, social and environmental levels,” adds Satel, who is the coauthor of Brainwashed: The Seductive Appeal of Mindless Neuroscience, a 2013 book about the real-world perils of neurotechnologies.
Satel is concerned that if the brain disease perspective takes hold of America, it could drive out alternative forms of comprehensive treatment. “That would be a real shame—a real tragedy—because I think we have medicalized the addict out of addiction,” she says. “But the problem is you can’t treat addiction out of a doctor’s office. After all, we are having the worst opioid crisis in the history of this country and the brain disease model didn’t keep us out of it.”
The brain disease framework has its origins in the early 1990s, when functional magnetic resonance imaging (fMRI) of the human brain was introduced to the world. Based on selective, narrow studies, it implies—erroneously, in the view of critics—that the brain is necessarily the most important and useful level of analysis for understanding and treating addiction. Addicts are often portrayed as helpless victims of their “hijacked brains” instead of people who have choices, particularly the capacity to respond to incentives.
BIG MEDICINE
Partly in response to the nonmedical epidemic surrounding prescription opioids, which prompted President Donald Trump in March to establish a commission on combating the public health crisis, the medical establishment has thrown its weight behind the MAT concept of treating addiction.
The campaign gathered steam in 2011, when 10 medical institutions in eight states, including New York, Massachusetts and Florida, introduced the nation’s first accredited residency programs in addiction medicine for general practitioners. Previously, the programs had been heavily targeted at psychiatrists. Now, all of a sudden, physicians newly out of medical school were being encouraged to study the connection between brain chemistry and addiction to substances ranging from alcohol and drugs to pharmaceutical medicines and nicotine.
Another major step toward the growing medicalization of addiction occurred in 2013, when the American Psychiatric Association issued its fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) after a span of 19 years. Psychiatry’s “bible” for diagnostics, which insurance companies rely on for billing treatments, dropped the use of two long-running umbrella terms—“substance abuse” and “substance dependence”—replacing them with no less than six “substance use disorders.” The new maladies run the gamut from “alcohol use disorder” and “cannabis use disorder” to “stimulant use disorder,” “hallucinogen use disorder” and “opioid use disorder.” Even “tobacco use disorder” made the list.
Revision of the manual, which includes hundreds of disorders, sparked fears that not only would the changes to the definitions of conditions sharply boost the number of people diagnosed with disorders, but they would add hundreds of millions of dollars in healthcare expenses—to benefit the medical, psychiatric and insurance industries.

After all, DSM panel members have deep ties to pharmaceutical companies. University of Pennsylvania psychiatrist Charles P. O’Brien is a prime example. He headed the group of researchers that revised the Diagnostic and Statistical Manual’s addiction standards and has been a consultant for Big Pharma firms including Pfizer, GlaxoSmithKline and Sanofi-Aventis, all of which manufacture anti-addiction drugs. Another Pharma company that has paid him for extensive consultant work is Alkermes, which was developing a drug designed to block cravings for alcohol and heroin. Of note, O’Brien was instrumental in getting “cravings” added to the symptoms for addiction listed in the DSM. O’Brien’s view on addiction drugs could not have been more unequivocal. “It’s unethical not to use medications,” he was quoted as stating in a 2011 issue of Addiction Professional, a magazine published by the Institute for the Advancement of Behavioral Healthcare, which claims to be “the leading education provider to behavioral healthcare professionals.”
Then in November 2016, U.S. Surgeon General Vivek Murthy called for a change in the way the nation addresses substance addictions. In his office’s first-ever assessment of the devastating $442 billion annual impact of alcohol and drugs on the nation’s health, Murthy made an impassioned plea for the increased use of medication in tackling addiction, urging Americans to embrace “a cultural shift” in how they think about addiction.
“For far too long, too many in our country have viewed addiction as a moral failing,” he said. “We must help everyone see that addiction … is a chronic illness that we must approach with the same skill and compassion with which we approach heart disease, diabetes and cancer.”
The latest evidence of the medicalization of addiction came on January 16, 2017, from the White House Office of National Drug Control Policy, the nation’s top policy-making agency tasked with eradicating illicit drug production and its trafficking and use, while monitoring drug-related national health outcomes. In a Web-based seminar titled “Medication-Assisted Treatment in Prisons and Prison Reentry Programs,” the agency applauded the “good work” done over the preceding year in making MAT available to addicted inmates in federal and state prisons.
The presentation marked a significant departure from government policy as recently as two years ago, when any medication-based treatments for addiction were forbidden by law in federal prisons. Various presenters proclaimed that MAT is now “the standard of care for opioid use disorder” and that “opioid addiction is an often-fatal brain disease.” The statements highlighted the continuing expansion of the medicalization of addiction in America.
The most disturbing aspect of the briefing was an assertion that any correctional institution that denies prisoners access to MAT would be in violation of the Americans with Disabilities Act, the Rehabilitation Act, and possibly the Eighth and Fourteenth Amendments of the U.S. Constitution, which respectively revolve around “cruel and unusual punishments” and “citizenship rights and equal protection of laws.”
The use of anti-discrimination laws to enforce MAT in prisons has already resulted in at least one unintended consequence: In Maryland, which suffers from some of the highest rates of drug addiction and alcoholism in the nation, drug-free addiction treatment programs that refuse to accept patients using MAT are being denied subsidized state funding.
Of all the federal government entities that helped perpetuate what psychiatrist Sally Satel refers to as a “noble lie,” perhaps none bears more responsibility than NIDA, one of the 27 institutes and centers comprising the National Institutes of Health (NIH), the nation’s premier medical research agency.
“The NIH is a biomedical agency, and NIDA wants to fit in,” Satel explains. “So the more NIDA focuses on the neuroscience of addiction, brands it and pushes it, the more consistent the agency seems with the mission of a biomedical institution.”
BIG PHARMA
The ideological engine behind the brain disease model of addiction is a partnership of sorts in which Big Medicine provides the scientific legitimacy and Big Pharma helps push the message along—sometimes with the help of high-profile Washington politicians.
That is precisely what happened in June 2016 when former Republican House Speaker Newt Gingrich, former Democratic Congressman Patrick Kennedy and Van Jones, a one-time CNN commentator and aide to former President Barack Obama, jointly authored a Time magazine opinion column aimed at addressing the opioid epidemic.
Titled “Treat America’s Opioid Epidemic With Medication,” the article was of a piece with numerous other blatantly partisan attempts to justify MAT. It argued, for example, that “like diabetes and asthma, [addiction is] not likely to be beaten by sheer willpower, but must be managed and treated like any other chronic disease.” The U.S. Centers for Disease Control, the article continued, “found that traditional forms of treatment tend to fail: Eighty percent or more of those in treatment for addiction will relapse.”

Media investigations subsequently revealed that both Gingrich and Kennedy are paid advisors to Advocates for Opioid Recovery, a nonprofit they helped launch in 2016. The organization is a strenuous advocate for increased government funding and insurance coverage for “science-based, evidence-based” opioid-addiction medication, not just as the standard for care but as a pathway to recovery.
According to further revelations, the organization is secretly funded by Braeburn Pharmaceuticals, a Princeton, New Jersey-based private company that won approval last year to market a brain implant that continuously dispenses the opioid addiction medication buprenorphine. The prescription drug, along with methadone, is one of the key medication-assisted treatments for detoxification from heroin.
In January, Braeburn reportedly disclosed to the Securities Exchange Commission that it had entered into an agreement with a private equity firm that owns the drugmaker to pay a $900,000 charitable donation to Advocates for Opioid Recovery. Braeburn indicated that it had already paid $675,000 to the nonprofit.
Kennedy is closely tied to addiction treatment centers that stand to benefit from the increased use of—and wider insurance coverage for—MAT. What’s more, a string of treatment centers that use MAT are sponsors of the Kennedy Forum, a nonprofit group Kennedy founded to boost treatment access for people suffering from mental illness and addiction, besides promoting research in the field.
One of the organizations sponsoring the Kennedy Forum is CleanSlate Addiction Treatment Centers, on whose board Kennedy sits. The organization reportedly paid $750,000 in 2016 to settle government allegations that it had improperly prescribed Suboxone, a prescription medicine used to treat adults addicted to opioids, whether illegal or not. Suboxone is one of the medications advocated by Kennedy, Gingrich and Jones.
“The big danger for the field of addiction medicine as it becomes recognized is that it, too, will engage in the kind of pill pushing that has played such a big role in the opioid crisis.”
As if all that weren’t enough to suggest that the unlikely trio of Kennedy, Gingrich and Jones had more than a vested interest in tackling the opioid crisis, they have been accused of providing a narrowly skewed meta-analysis of 19 studies that they cited to back up their support for MAT.
The subjects in the studies “often do not resemble the general population of treatment seekers,” according to Jason Schwartz, clinical director of Dawn Farm, a respected residential addiction treatment center in Michigan. The studies also paid very little attention to abstinence from drugs on the part of subjects, notes Schwartz in “Addiction and Recovery News,” a blog he writes.
Perhaps the most publicly visible display of Big Pharma’s political connections in recent memory occurred this past December, when, in a 94-5 vote, the U.S. Senate approved the “21st Century Cures Act,” one of the largest bills ever aimed at reforming the FDA. The $6.3 billion law, which President Obama signed before leaving office, calls for greater use of MAT and includes $1 billion for opioid prevention and treatment programs in 50 states over two years.
“This final deal has only a tiny leaf of funding for NIH and for the opioid crisis,” remarked Democratic Senator Elizabeth Warren, shortly before the bill’s passage. “Why pretend to give money to NIH or opioids?” she asked, adding: “Because this funding is political cover for huge giveaways to giant drug companies.”
The federal government’s minimal constraints on Big Pharma’s aggressive marketing methods and sales of prescription drugs raises serious questions about MAT. “The big danger for the field of addiction medicine as it becomes recognized is that it, too, will engage in the kind of pill pushing that has played such a big role in the opioid crisis,” says Anna Lembke, chief of addiction medicine at the Stanford University School of Medicine.
The author of the critically acclaimed 2016 book, Drug Dealer, MD: How Doctors Were Duped, Patients Got Hooked and Why It’s So Hard to Stop, Lembke points out that although the pharmaceutical industry, particularly the manufacturers of opioid painkillers such as OxyContin, has played a big role in the opioid epidemic, it would be a mistake to ascribe all the blame to Big Pharma.
Pharmaceutical companies were successful in getting doctors to over-prescribe opioids because of the industry’s ability to team up with physicians in academia, professional medical societies, regulatory agencies and the FDA, says Lembke. Together, these different factions, the “House of Medicine,” as Lembke likes to call them, “manipulated and misrepresented, deliberately or otherwise, medical science to serve their own agendas.”
Given the momentum behind MAT, not to mention the support it enjoys among members of the nation’s medical, commercial and political elite, addiction may yet be destined to endure as one of the world’s least understood and mistreated social maladies.