In 2009, the Government Accountability Office (GAO), a federal agency that provides auditing, evaluation and investigative services for Congress, set a key deadline for the Food and Drug Administration (FDA). Specifying an eight-month target date, the GAO instructed the FDA to ask U.S.-based manufacturers of high-risk medical devices to furnish proof of their safety and efficacy as well as information about their adverse effects.
Among those devices was the electroconvulsive therapy (ECT) machine, which the FDA has deemed potentially dangerous since 1976, the year the agency first became responsible for regulating not just everything from bottled water to diet pills, but every medical device sold in the nation. Nearly 10 years later, ECT manufacturers have yet to furnish the evidence that the GAO demanded. Similar demands for evidence of safety and efficacy of the machines were made by the FDA to ECT device manufacturers in 1979 and again in 1990. The manufacturers failed to comply and the FDA did not enforce its directives.
How ECT manufacturers and the FDA have been able to thumb their noses at one of the nation’s most respected agencies is a story riddled with conflicts of interest that can surprise even the most dogged investigator.
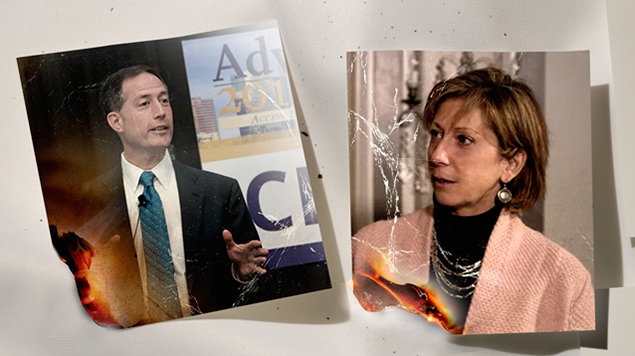
In January 2010, almost exactly a year after the GAO asked for proof of the safety and effectiveness of medical devices on the market, Jeffrey E. Shuren, an official who had held various policy and planning positions at the FDA, became director of the agency’s Center for Devices and Radiological Health (CDRH). It just so happened that Shuren’s wife, Allison Shuren, was—and still is—a partner at the Washington, D.C. office of the law firm Arnold & Porter, where she co-chairs the firm’s FDA/healthcare practice group.
“The FDA has always treated shock machines differently from all other medical devices.”
National Association of Rights Protection and Advocacy
If the implications of that snug marital relationship for the medical industry aren’t clear, this is where the conflict of interest goes up another notch: Arnold & Porter, under the co-chairmanship of the FDA’s director’s spouse, represents medical device makers as well as a range of pharmaceutical and biotech companies. What’s more, one of Allison Shuren’s law partners, William Vodra, is an expert on regulatory issues regarding the safety, effectiveness and marketing of medical products, including medical devices.
Vodra was a member of a committee of the Institute of Medicine (the organization changed its name earlier this year to the Health and Medicine Division of the National Academies of Sciences, Engineering and Medicine), which was charged with reviewing the so-called 510(k) process, a critical component of FDA review named after a section of the Federal Food, Drug and Cosmetic Act. Devices that the FDA deems to have a low risk to patients generally can be sold if they are cleared through the 510(k) process, which allows the agency to approve products without clinical tests as long as manufacturers can show that they are substantially similar to another legally marketed device. High-risk devices however are required to pass clinical trials proving safety and effectiveness before they can be approved by the FDA for use.
In 2011, speaking before the U.S. Senate Committee on Health, Education, Labor and Pensions, Jeffrey Shuren vigorously and successfully defended the 510(k) process for approving medical devices, whose U.S.-based manufacturers, he proudly claimed, dominate the roughly $350 billion global medical device industry. A number of flaws in the process, Shuren declared, had been fixed, following a re-evaluation and modernization of the agency’s regulatory review process. Its goal, he added, is not “more regulation or less regulation” but “smart regulation.”
Shuren, who declined to be interviewed for this article, did not elaborate on what he meant by “smart regulation.” But it’s probably fair to say that he was being too clever by half. That’s because when the FDA issued a “proposed order” in December 2015 that it would downgrade ECT devices from high-risk to low-risk, largely because of decades-long pressure by the American Psychiatric Association (APA)—by far ECT’s biggest supporter—many health reform critics and former shock therapy patients were furious. Although ECT machines have been in use since the FDA began regulating medical devices in 1976, it has never passed the standard for high-risk devices—through science based clinical trials.
“It would be unprecedented for the agency to declare a device safe without any submission of safety data from its manufacturers, but the FDA has always treated shock machines differently from all other medical devices because of the power of the APA,” said the National Association of Rights Protection and Advocacy, an organization that informs and mentors individuals diagnosed with psychiatric illnesses to make their own treatment choices, in an online primer on the FDA’s role in pushing for ECT’s increased use despite the near-total absence of clinical data about its value.
The relationship between the medical device industry and the FDA’s Center for Devices and Radiological Health runs deep. According to memos obtained by Inside Health Policy through a Freedom of Information Act request, FDA officials met privately with representatives of AdvaMed, a medical device industry trade association, which reportedly spent $2.3 million lobbying Congress in 2014 to discuss the text for the 21st Century Cures Act. The legislation, which passed the House in July 2015 and is pending consideration in the Senate, focuses on fast-tracking FDA’s approvals of “innovative” medical devices and drugs. Health advocates are concerned that if the legislation becomes law, the standard for approval of high-risk medical devices will be lowered.
Further, according to an August 7, 2015 FDA memo obtained by Inside Health Policy, CDRH officials met with AdvaMed executives to settle on “the proposed language for most of the device provisions” in the legislation. The meeting was attended by Jeffrey Shuren, then-acting FDA Commissioner Stephen Ostroff and present-day FDA Commissioner Robert Califf, a former Duke University cardiologist with long-standing financial and clinical trial ties to pharmaceutical companies. Others at the table included executives from Johnson & Johnson and St. Jude Medical Inc., a Minnesota-based global medical device company that in 2014 failed two major depression treatment trials for a deep brain stimulation device that the FDA has approved as an experimental treatment for depression.